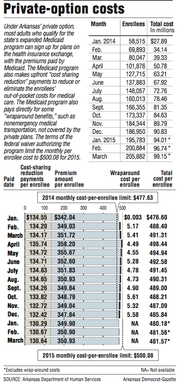
The per-person payments to insurance companies for coverage under Arkansas' private-option Medicaid program rose by about 1 cent this month to $481.57, according to the state Department of Human Services.
The Human Services Department paid the companies $99.1 million on behalf of 205,882 Arkansans who had completed enrollment as of Feb. 15, department spokesman Amy Webb said in an email.
That payment included an average monthly premium of $350.93 and an average of $130.64 in subsidies, known as cost-sharing reduction payments, that are meant to reduce or eliminate enrollees' out-of-pocket expenses for medical care.
Compared with the payments for February, the individual premium for March was about 3 cents higher, while the average cost-sharing payment was about 2 cents lower.
It was the second-straight month that the average enrollee payment to the insurance companies has increased. But the amount for March remains below a monthly cost target of $500.08 set for 2015 in the federal waiver authorizing the program.
Webb has said the monthly costs are expected to fluctuate but remain well below the cost target for this year.
Sen. David Sanders, R-Little Rock, a sponsor of the law creating the private option, called the monthly cost numbers "encouraging" and something lawmakers should take into account as they explore alternative coverage options.
Sanders noted that the expanded Medicaid program has been credited with holding down the premiums for plans available on the exchange to those who don't qualify for Medicaid-funded coverage.
"The key question is are we learning valuable lessons from the private option, and I think the answer is yes," Sanders said. "We're showing that a large-scale premium assistance program for low-income individuals can work, as opposed to just sticking them on straight Medicaid, and we're showing that it can have positive impact on the marketplace."
Under the private option, the state Medicaid's program buys coverage on Arkansas' health insurance exchange for adults with incomes up to 138 percent of the poverty level: $16,105 for an individual, for instance, or $32,913 for a family of four.
The state created the program in 2013 as a primary way to expand Medicaid coverage as authorized under the 2010 Patient Protection and Affordable Care Act.
Adults who are deemed to have exceptional health needs, making up about 10 percent of those made eligible under the expansion, are covered under the traditional, fee-for-service Medicaid program.
An Arkansas legislative task force is studying options for replacing the private option in 2017, when a federal waiver authorizing the program expires and Arkansas will be required to begin paying a portion of the cost.
In the meantime, the federal government is expected to pay the full cost of the program through 2016 as long as the cost stays below a cap that will be calculated using the monthly per-enrollee cost targets.
If the state's costs are above the cap at the end of the three-year demonstration period, the state will owe the difference to the federal government.
Last year, the monthly cost averaged $489.70 per enrollee -- more than $12 above the 2014 target. But Human Services Department officials have said they expect this year's costs to be low enough that they will more than make up for last year's.
The cost target for next year rises to $523.58.
Last year's cost included an average of $4.91 per enrollee for so-called wraparound benefits, such as nonemergency medical transportation, that must be provided under federal Medicaid rules but aren't covered by the private plans. The state Medicaid program pays for those services directly.
Information on wraparound costs for January and February wasn't available on Thursday.
Premiums, which are set by the insurance companies and approved by state and federal officials, vary according to the plan an enrollee selects and the enrollee's age, with higher premiums charged for older enrollees.
Cost-sharing reduction payments are lower for enrollees with incomes above the poverty level because they are required to make some co-payments -- $8 for a doctor's office visit, for instance -- or contribute up to $15 per month to help pay the cost of their medical care.
Metro on 03/27/2015